Value based healthcare is the buzzword in healthcare worldwide. Inspired by Harvard professor Michael Porter’s legacy, initiatives have been taken around the world, in order to achieve high quality care at lower costs. These are splendid objectives. However, is Value Based Healthcare (VBHC) really the new panacea within the healthcare sector that will deliver true value for patients? Or is it a pseudo-innovation, i.e. a renovation-oriented approach?
The renovation hype
In recent years, commercialization of healthcare has lead to an increased interest in management theories. However, management concepts appear to be sensitive to trends. We have only just mastered Lean Six Sigma, and already we have to start working with VBHC. This is called pseudo-innovation: ‘The redefining of similar ideas and methods every 3 to 5 years, using new words.’ As a consequence, initiatives for improvement are not given enough time and opportunity to be embedded in everyday practice. They exist as management toys, or even worse, they infect staff dreading the umpteenth improvement programme with the ‘projectitis’ virus.
When the solution is the problem
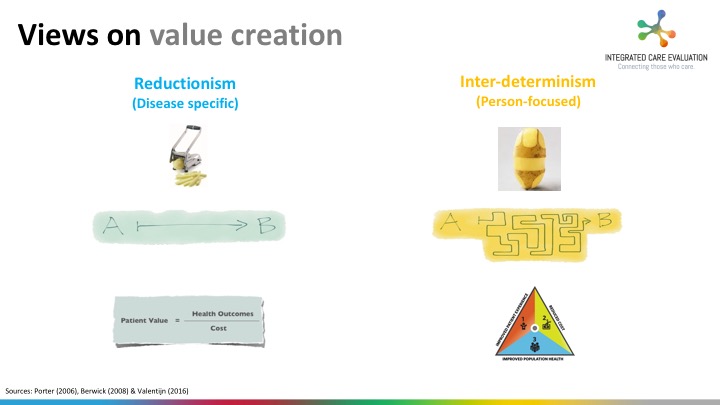
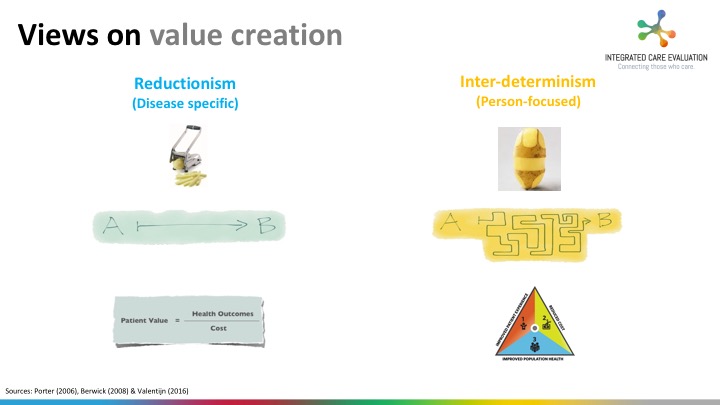
VBHC and Triple Aim – defined as improved patients’ experience of care, population health, and reduced costs per capita – are often uttered in the same breath, yet they are two different views on the method of value creation. VBHC is based on a disease-oriented approach based on competition in value, in which value is defined as: the health outcome per dollar euro spent. Compare this to Triple Aim, which focuses more on a broad people-oriented and population-oriented approach. VHBC is especially in use in secondary healthcare, whereas Triple Aim is more common in primary healthcare and public health.
No integration, no value creation
There is one thing perfectly clear in the discussion on VHBC and Triple Aim: improved health outcomes per dollar spent can only be achieved through constructive partnerships across the entire care continuum (including health promotion, prevention, social care, and healthcare). In other words, the integration of services to improve health outcomes. Research shows that functional (linear) thinkers as well as normative (systems) thinkers require preconditions in order to make our healthcare sustainable future-proof. To put it plainly, spreadsheet management and outcome-based financing supplemented by a solid change management approach are needed to make a difference.

Around the world, healthcare is grinding to a halt as involved parties hold on to their own domains and fight tribal wars. VBHC and Triple Aim supporters alike point out the need for integration across the entire care continuum. It is precisely this that demands an innovative approach by all the stakeholders involved. Unfortunately, healthcare is still compartmentalized, and therefore involved parties are unable to define and achieve objectives together. We can use a model like VBHC or Triple Aim if we like, but if we do not change the foundation and our attitude, we will remain stuck in renovation programmes.
There are no simple solutions
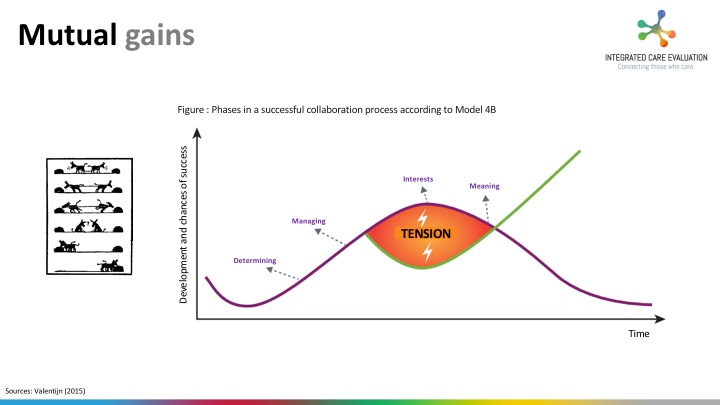
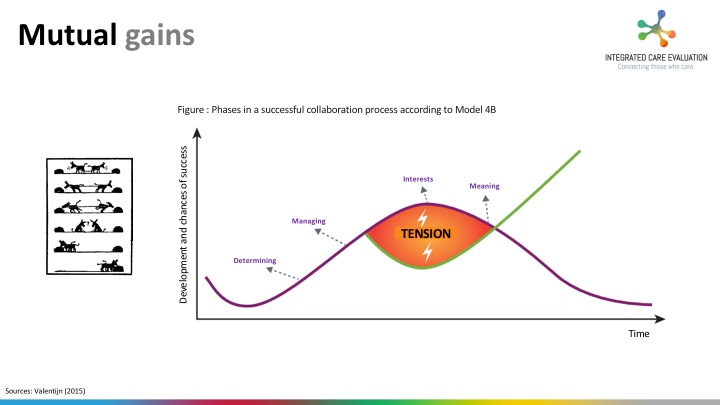
As it is proven difficult to clarify the interests of all involved parties, we will continue going around in circles, and will define the situation as a complex problem within a complex system, finding it difficult to voice our true interests and those of our organizations. We have become really good in talking about barriers. However, precisely this clarification of mutual gains and collaborative advantage is necessary for a successful integration of care. Besides, there are no simple solutions to complex problems.
Walk the talk!
What is needed instead? To put it plainly: Walk the talk! All parties should work together in a constructive manner, without staring at problems and looking for solutions and mutual gains instead. By looking into best practices in, for example, Germany, the United States, United Kingdom, Sweden and Australia. By learning how these initiatives can achieve better outcomes at lower costs through integration of care. Let us try to apply these principles in their own contexts. And let us refrain from reinventing the wheel. Let us work together on an integral business case, instead of pointing the finger at each other and complaining about the lack of money. It is time that we explore new routes, and set up constructive, cooperative collaborations. And yes, patients, healthcare providers and board members should all be involved. Only then, will we start to innovate.
Will you join us?
I hope that the insights we have mentioned in this article will inspire you to turn VBHC into an innovative approach in 2017. We would like to share our knowledge in order to put this into practice. Take a look around on www.integratedcareevaluation.org to find out how we can help you.
Integrated Care Evaluation
Connecting those who care
 Understanding how integrated delivery and payment models are being implemented is key in an era of value-based healthcare. Integrated care can be compared to a black box that may, or may not provide the ‘out of the box’ solutions needed to help improve patients’ care experiences and health, and to minimise costs. One of the challenges in bringing theory into practice is the lack of a universally accepted method for measuring integrated care. This poses significant challenges for policymakers, commissioners, managers, professionals and researchers to support the effective deployment and evaluation of integrated care in daily practice.
Understanding how integrated delivery and payment models are being implemented is key in an era of value-based healthcare. Integrated care can be compared to a black box that may, or may not provide the ‘out of the box’ solutions needed to help improve patients’ care experiences and health, and to minimise costs. One of the challenges in bringing theory into practice is the lack of a universally accepted method for measuring integrated care. This poses significant challenges for policymakers, commissioners, managers, professionals and researchers to support the effective deployment and evaluation of integrated care in daily practice. The International Foundation of Integrated Care and Integrated Care Evaluation would like to tap into your knowledge, experience, and expertise in the field of integrated care and invite you to take part in a cross-national study. As we aim to present the results at the upcoming International Conference on Integrated Care in Utrecht, the Netherlands, we hope you can free up some time to participate.
The International Foundation of Integrated Care and Integrated Care Evaluation would like to tap into your knowledge, experience, and expertise in the field of integrated care and invite you to take part in a cross-national study. As we aim to present the results at the upcoming International Conference on Integrated Care in Utrecht, the Netherlands, we hope you can free up some time to participate.